Source images: Julia Kozlov/iStock; Yevheniia Bunha/iStock
Imagine: You're conscious on the operating table, your mouth is full of tubes, and the surgeon is wondering, "How does it feel?" Possible answers: painfully grimace or heroically shake your head. Both are lies. Fortunately, a team of scientists from Germany has decided to put an end to this theater of the absurd and entrust the assessment of pain to a machine that does not believe your winks. Their method? A non-contact lie detector based on a camera and AI that analyzes what you carefully hide: your face and heart.
Ingenious and simple: if the patient can't say "ouch," the algorithm will tell him.
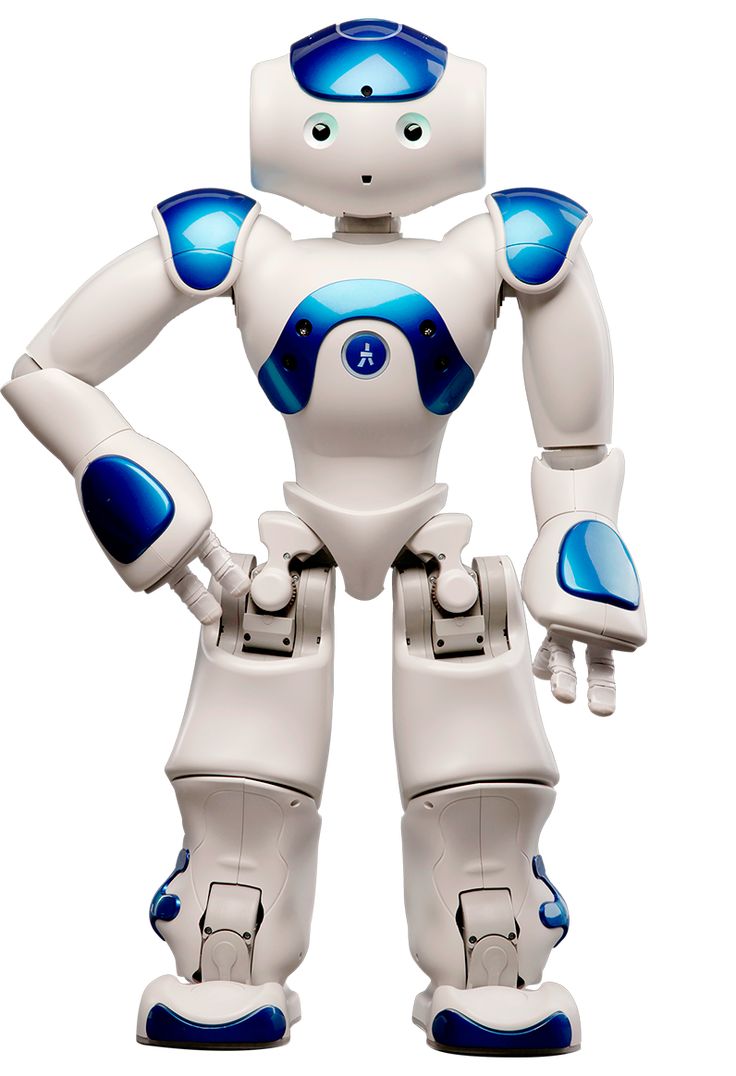
The problem of an anesthetized but conscious patient is a headache for anesthesiologists. Infants, patients with dementia, or just people who have fallen into a postoperative stupor — they all become "black boxes" for doctors. Existing methods like ECG electrodes are cumbersome and interfere with work. German researchers led by Bianca Reichardt have proposed an elegant solution: a conventional camera and a smart algorithm.
The system works in two stages, like an experienced investigator.:
*Video Interview: The AI meticulously studies the slightest changes in facial expressions, from barely noticeable eyebrow twitching to lip biting.
Lie Detector: Using the rPPG technology, the camera measures the heart rate by changing skin color. The algorithm analyzes seven key parameters, including pulse maxima and minima, a direct physiological clue that cannot be hidden.
"This eliminates the need to tape the patient with sensors," Reichard notes dryly. Finally, progress: instead of a web of wires, there is only the evil glass eye of the camera, dispassionately recording your discomfort.
Realism training: Why 45% accuracy is (almost) a victory
And this is where the fun begins and the reason for healthy skepticism. The accuracy of the model was only 45%. "Total" is when compared with other laboratory algorithms that break records on perfect five—second videos with good lighting. But the German team is apparently full of masochistic idealism.
They deliberately trained AI on "dirty" data: long (up to 3 hours) recordings of real operations, where the light blinks, the camera shakes, and the patient's face is half hidden by a mask or surgeon. "This reflects a more realistic clinical situation," says Reichard. That is, their AI is not a child prodigy at the sterile Olympics, but a seasoned fighter who was thrown into the trenches of real medicine. And his modest 45% looks much more honest in these conditions than 95% in greenhouses. The author himself is surprised that the algorithm even saw something through this chaotic flickering.
The future: pain under control, or How not to become a guinea pig
What's next? The accuracy will be improved by making the models more complex. But the real charm is in the scale. Imagine a network of such cameras in an intensive care unit, where one doctor monitors dozens of patients. The algorithm quietly monitors everyone's condition and sounds the alarm when the pain goes beyond the acceptable range. This is no longer just a gadget, but a part of the hospital ecosystem, where technology quietly and tirelessly keeps its watch. Such complex systems are the future of automation, where every device, from the camera to the analyzer, performs its task. Perhaps one day their work will be controlled by advanced dispatch platforms similar to those that are being developed within the framework of the concept JOBTOROB.com, which deals with the optimal distribution of tasks between autonomous systems.
So get ready. Soon, your pain will be assessed not by shouting, but by an algorithm. And maybe that's for the best. After all, you can't lie to a car that "everything is fine" just to get rid of it as quickly as possible.