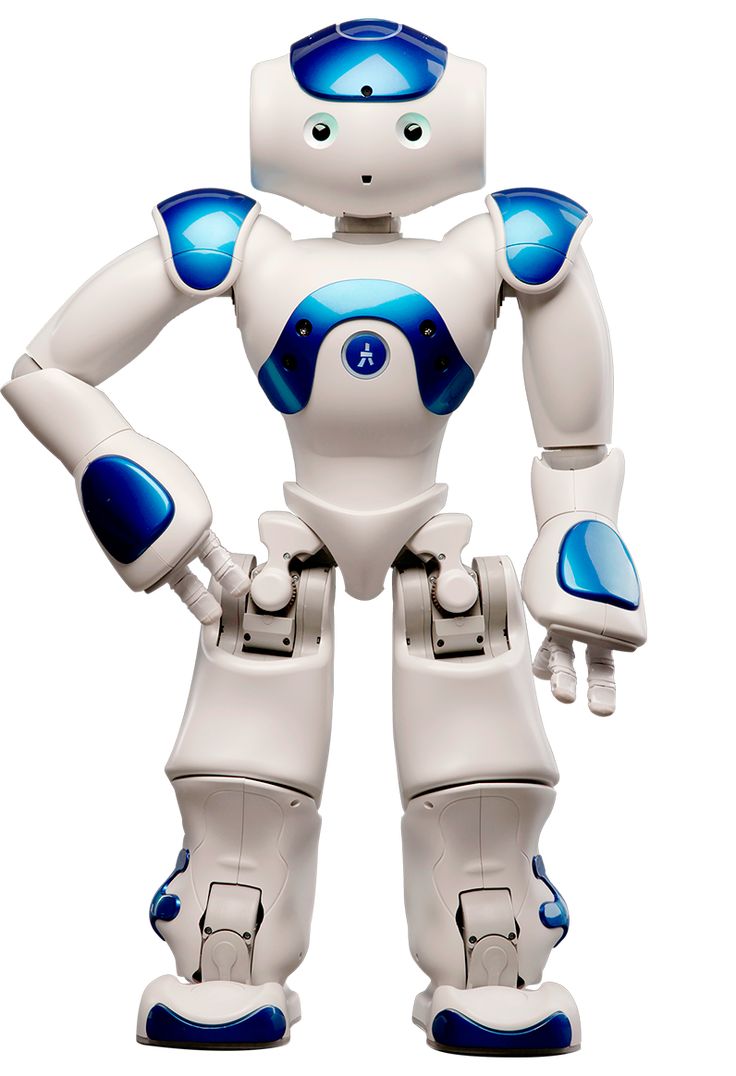
In a groundbreaking development that promises to revolutionize the field of prosthetics, researchers from MIT and Brigham and Women's Hospital have achieved a milestone in restoring natural walking abilities to individuals with lower limb amputations. This innovative approach, detailed in a recent study published in Nature Medicine, marks the first time in history that a prosthetic leg has been successfully operated under full neural control, resulting in a biomimetic gait that closely mimics natural human movement.
The Power of Neural Reconnection
At the heart of this advancement is a novel surgical technique known as the agonist-antagonist myoneural interface (AMI). Unlike traditional amputation procedures that disrupt the natural pairing of muscles responsible for limb movement, the AMI surgery reconnects these muscle pairs within the residual limb. This reconnection preserves the dynamic communication between muscles, allowing the nervous system to accurately sense muscle position and contraction speed – crucial information for the brain to control limb movement effectively.
Hugh Herr, a professor of media arts and sciences at MIT and senior author of the study, emphasized the significance of this achievement: "This is the first prosthetic study in history that shows a leg prosthesis under full neural modulation, where a biomimetic gait emerges. No one has been able to show this level of brain control that produces a natural gait, where the human's nervous system is controlling the movement, not a robotic control algorithm."
Study Design and Remarkable Outcomes
The research team, led by postdoctoral researcher Hyungeun Song, conducted a comparative study involving seven individuals who had undergone the AMI surgery and seven with traditional below-knee amputations. All participants were fitted with the same type of bionic limb, featuring a powered ankle and electrodes capable of detecting electromyography (EMG) signals from specific muscles.
Subjects were put through a series of challenging scenarios, including level-ground walking, navigating slopes and stairs, and avoiding obstacles. The results were striking: AMI patients consistently outperformed their counterparts with traditional amputations. They walked faster – at speeds comparable to non-amputees – and demonstrated more natural movements, such as pointing their prosthetic toes upward when climbing stairs or stepping over obstacles.
Perhaps most impressively, these improvements in gait and mobility were achieved with less than 20% of the sensory feedback typically available to individuals without amputations. This finding underscores the remarkable adaptability of the human nervous system and the potential for even minor increases in neural feedback to dramatically enhance prosthetic control.
Beyond Mobility: Psychological and Physical Benefits
The benefits of the AMI procedure extend beyond improved mobility. Patients reported experiencing less pain and reduced muscle atrophy following the surgery. These outcomes suggest that the AMI approach not only enhances functional capabilities but also contributes to improved overall well-being for individuals living with limb loss.
Dr. Matthew Carty, a surgeon at Brigham and Women's Hospital and co-author of the study, highlighted the collaborative nature of this advancement: "This work represents yet another step in us demonstrating what is possible in terms of restoring function in patients who suffer from severe limb injury. It is through collaborative efforts such as this that we are able to make transformational progress in patient care."
A Paradigm Shift in Prosthetic Design
This research signals a potential paradigm shift in the approach to prosthetic development. While recent years have seen significant advancements in robotic prosthetics with sophisticated sensors and controllers, these devices often rely on predefined algorithms rather than direct neural control. The AMI approach, in contrast, aims to create a more intuitive and embodied experience for users.
Professor Herr articulated this vision: "The problem with that long-term approach is that the user would never feel embodied with their prosthesis. They would never view the prosthesis as part of their body, part of self. The approach we're taking is trying to comprehensively connect the brain of the human to the electromechanics."
Looking Ahead: Implications and Future Directions
As of now, approximately 60 patients worldwide have received the AMI surgery, with applications extending to arm amputations as well. The success of this study opens up exciting possibilities for further research and development in the field of neuroprosthetics.
Future studies may explore ways to further enhance neural feedback and control, potentially leading to even more natural and intuitive prosthetic use. Additionally, the principles underlying the AMI approach could inform advancements in other areas of medical technology, such as neural interfaces for various medical conditions.
The achievements outlined in this study represent a significant step towards realizing the dream of fully integrated, neural-controlled prosthetics that function as seamless extensions of the human body. As research in this field continues to progress, we may be witnessing the dawn of a new era in which the line between human and machine becomes increasingly blurred, offering hope and improved quality of life for millions of individuals living with limb loss worldwide.